Diverticulitis can affect our bodies in many ways, including causing back pain. Many people don’t know how this digestive issue can lead to discomfort in the lower back. We will look into how diverticulitis and back pain are connected, helping to clear up any confusion.
Key Takeaways
- Diverticulitis can cause referred pain to the lower back due to the anatomical connection between the colon and the spine.
- Back pain is a common symptom of diverticulitis, experienced by a significant number of patients.
- Proper diagnosis and treatment of diverticulitis are crucial to alleviate both abdominal and back pain.
- Lifestyle modifications, such as a high-fiber diet and regular exercise, can help prevent and manage diverticulitis-related back pain.
- Seeking medical attention for persistent or severe back pain, specially when accompanied by other digestive symptoms, is important for identifying the underlying cause.
What is Diverticulitis?
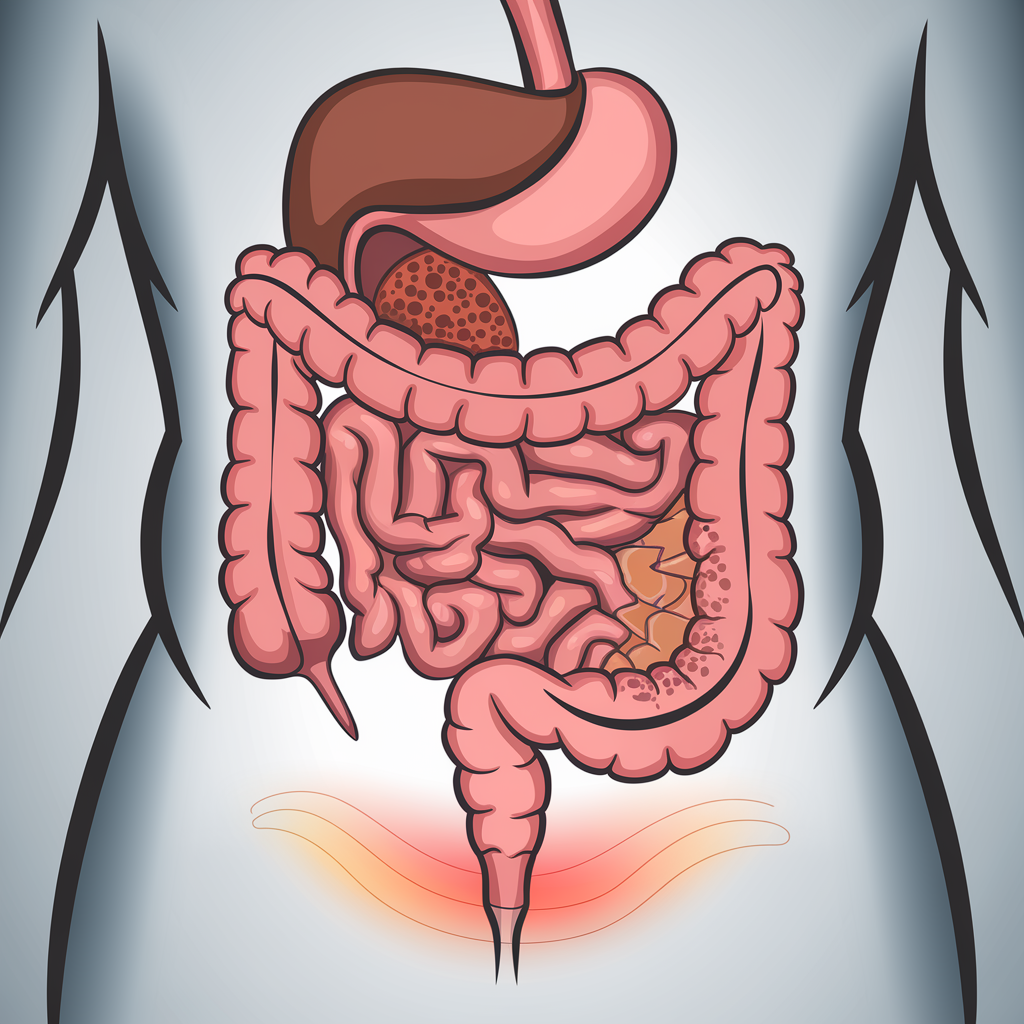
Diverticulitis is a condition where small pouches in the digestive system, usually in the colon, get inflamed or infected. This is a common problem, affecting about 50% of adults over 60 in the United States.
Understanding Diverticulitis and Its Causes
These pouches, called diverticula, form when the colon wall weakens. This allows the inner lining to bulge out. Experts think a low-fiber diet and constipation are the main reasons for this.
When these pouches get inflamed or infected, it causes diverticulitis. This condition can lead to pain, changes in bowel habits, and even serious complications like bowel obstruction or perforation.
- Diverticulosis affects up to 50% of adults over 60 in the United States.
- A low-fiber diet and constipation are the main risk factors for developing diverticulosis.
- When the diverticula become inflamed or infected, it leads to the painful condition of diverticulitis.
Knowing the causes and risk factors of diverticulitis is key to managing this common condition. By changing our diet and lifestyle, we can prevent diverticula and lower the chance of painful diverticulitis flare-ups.
Common Symptoms of Diverticulitis
Diverticular disease comes in two types: uncomplicated and complicated diverticulitis. When the pouches in the colon get inflamed, it causes a range of symptoms. Knowing the common symptoms of diverticulitis is key to managing it well.
Abdominal pain is a main symptom, often felt in the lower left abdomen. This pain can be sharp and severe or build up slowly. Other symptoms include fever, nausea, vomiting, changes in bowel habits, and tenderness in the abdomen.
Some people with diverticulitis may also have rectal bleeding, constipation, or diarrhea. These digestive problems can make the condition worse and affect daily life.
It’s important to remember that back pain is not a common symptom of diverticulitis. But, some may feel a dull ache in the back that gets worse with movement. This back pain is usually due to the inflammation in the colon, not the spine.
| Symptom | Description |
|---|---|
| Abdominal Pain | Sharp, severe pain in the lower left part of the abdomen during acute attacks or gradual buildup during chronic flare-ups. |
| Fever | Elevated body temperature, often accompanied by other symptoms of diverticulitis. |
| Nausea and Vomiting | Digestive discomfort and inability to keep food or liquids down. |
| Bowel Changes | Constipation, diarrhea, or alternating between the two. |
| Abdominal Tenderness | Sensitivity and discomfort when the abdomen is touched or pressed. |
| Rectal Bleeding | Bleeding from the rectum, which can be a sign of a more severe complication. |
| Back Pain | Constant, dull ache in the back that worsens with movement or pressure, often related to the colon inflammation. |
If you have any of these symptoms, get medical help right away. Early diagnosis and treatment can help manage the condition and prevent complications.
Can Diverticulitis Cause Back Pain?
Yes, diverticulitis can cause back pain. This happens because the colon and lower back are close and share nerves. When the colon’s pouches get inflamed, pain signals can go to the lower back.
This is called referred pain. It’s common when the lower colon is inflamed. The pain feels like it’s coming from the back, even though it starts in the abdomen.
It’s rare for diverticulitis to only cause back pain. Usually, people with it also have stomach pain, bloating, changes in bowel habits, and fever. Back pain is just one symptom.
Women, the elderly, and those with weak immune systems are more likely to feel back pain from diverticulitis. But how much pain and how often it happens can vary a lot.
If you have ongoing or mysterious back pain, see a doctor. They can figure out what’s causing it, including if it’s from diverticulitis.
Diverticulitis and Its Potential Complications
Understanding the Risks and Complications
Diverticulitis is a condition where the colon’s pouches get inflamed. If not treated, it can lead to serious problems. Most of the time, it’s not severe, but sometimes it can cause big issues.
Diverticular bleeding is a serious issue. The inflamed pouches can bleed, causing blood in the stool. This can make you feel pale, dizzy, and worried.
Intestinal obstruction happens when the colon swells and narrows. It can block the flow, causing pain, nausea, and vomiting.
Fistulas form when the pouches erode the colon walls. They create abnormal connections with other organs, like the bladder. This can lead to frequent urination and irritation.
Peritonitis is a severe complication. It happens when a pouch bursts, spilling contents into the belly. This can be life-threatening and needs immediate care.
Other issues include abscesses and gastrointestinal perforation. Abscesses might need to be drained, and perforation can cause sepsis if not treated.
About 15% of people with diverticulitis face complications. Risks grow with age, obesity, smoking, and a diet rich in red meat. A healthy lifestyle and quick medical care can help manage these risks.
| Complication | Description | Symptoms |
|---|---|---|
| Diverticular Bleeding | Severe inflammation causing the diverticula to bleed | Fresh blood in stool, paleness, dizziness |
| Intestinal Obstruction | Severe swelling and narrowing of the colon, leading to temporary or permanent blockages | Abdominal pain, nausea, vomiting |
| Fistulas | Abnormal connections between the colon and other body organs, such as the bladder | Frequent urination, irritation during urination |
| Peritonitis | Rupture of a diverticulum, allowing intestinal contents to spill into the abdominal cavity | Life-threatening infection, rigid and sensitive abdomen |
| Abscesses | Pockets of pus that may require drainage | Localized pain, swelling, and redness |
| Gastrointestinal Perforation | Rupture of the colon, leading to sepsis | Severe abdominal pain, fever, rapid heart rate |
It’s important to know about diverticulitis complications to get medical help quickly. A healthy lifestyle and working with doctors can help manage diverticulitis and lower the risk of serious problems.
Diagnosing Diverticulitis
Diagnosing diverticulitis involves a detailed process. It includes a physical exam, checking symptoms, and imaging tests. These steps help doctors confirm diverticulitis and rule out other causes of pain.
The first step is a thorough physical exam. Doctors check the abdomen for tenderness, often in the lower left. They look for signs of complications too.
Doctors also review symptoms like pain, fever, and changes in bowel habits. This helps them decide if it’s diverticulitis and what to do next.
Imaging Tests for Diverticulitis
To confirm diverticulitis, doctors use imaging tests. These include:
- Computed Tomography (CT) Scan: A CT scan is the best way to diagnose diverticulitis. It shows inflamed diverticula and any complications.
- Magnetic Resonance Imaging (MRI): An MRI might be used if a CT scan isn’t possible. It’s also used to check the colon and surrounding areas.
- Colonoscopy: A colonoscopy is done after the acute phase has passed. It helps check the colon for diverticula and other issues.
Early and accurate diagnosis is key for treating diverticulitis. Doctors use physical exams, symptom checks, and imaging to make a proper diagnosis. This ensures the right care for those with diverticulitis.
Treating Diverticulitis
Medical and Surgical Interventions
The treatment for diverticulitis varies based on how severe it is. For mild cases, doctors often use antibiotics, a liquid diet, and rest. This helps the inflamed pouches to heal. But, more serious or ongoing cases might need more help, like staying in the hospital for IV antibiotics and fluids.
For some, surgery is the next step. This could mean removing part of the colon or draining an abscess. The treatment plan depends on the patient’s symptoms, risk factors, and how they first respond to treatment.
It’s key to remember that antibiotics and rest might not work for everyone. Surgery is sometimes needed for severe or recurring diverticulitis, like when there are perforations, abscesses, or fistulas.
- Mild diverticulitis cases may be managed with a course of antibiotics, a liquid diet, and rest to allow the inflamed pouches to heal.
- Severe or recurring diverticulitis may require hospitalization for intravenous antibiotics and fluids.
- In some cases, surgery may be necessary to remove the affected portion of the colon or drain an abscess.
- The specific treatment plan will depend on the individual patient’s symptoms, risk factors, and response to initial treatment.
“Diverticulitis can be a challenging condition to manage, but with the right combination of medical and surgical interventions, we can often achieve positive outcomes for our patients.”

Diverticulitis and Diet
Diet is key in both causing and managing diverticulitis. Eating low-fiber foods can increase the risk of diverticulosis and flare-ups. On the other hand, enough fiber makes stool softer and reduces colon pressure, which helps prevent diverticula.
When you have diverticulitis, doctors might suggest a low-residue or liquid diet. This lets the colon rest and heal. It helps avoid further irritation to the inflamed or infected diverticula.
Studies show that up to 30% of people with diverticulosis will have a flare-up. By age 60, half of Americans have diverticula in their colon. The bright side is that a high-fiber diet can help prevent diverticulitis complications.
| Recommended Daily Fiber Intake | Amount |
|---|---|
| Women up to age 50 | At least 25g |
| Women over 50 | At least 22g |
| Men up to age 50 | At least 31g |
| Men over 50 | At least 28g |
Most Americans only get 10 or 15 grams of fiber daily, which is too little. Adding more fiber-rich foods to your diet can prevent diverticula and lower diverticulitis flare-up risks.
“Nutrition therapy for diverticulitis is a temporary measure to allow the digestive system to rest.”
It’s vital to gradually return to a diet with fiber once you’re better. A long clear liquid diet can lead to weakness and other issues due to lack of nutrients.
Prevention and Risk Factors
While we don’t know all the causes of diverticulitis, we do know some risk factors. Knowing these can help us prevent the condition.
A low-fiber diet is a big risk factor. People who eat more fiber have a 40% lower risk of diverticulitis problems. Eating fruits, veggies, and whole grains can help prevent diverticula and lower the risk of diverticulitis.
Age is also a big risk factor. By 40, 5% of people have diverticula. By 80, it’s at least 50%. As we get older, the risk of diverticulitis goes up, with symptoms often showing in those over 70.
Some medications, like NSAIDs and steroids, can also raise the risk. These can mess with the digestive system, leading to diverticula and complications.
Lifestyle factors like obesity, not being active, and smoking also increase the risk. Staying healthy, exercising, and quitting smoking can help prevent diverticulitis.
Knowing these risk factors and making lifestyle changes can help prevent diverticulitis. Regular health check-ups can also help find and manage health issues that raise the risk.
Living with Diverticulitis
Managing Chronic Diverticulitis and Quality of Life
For some, chronic diverticulitis is a long-term issue. It can be hard to manage flare-ups and keep a good quality of life. But, with the right help and strategies, it’s possible to manage symptoms and feel better.
Changing your diet, taking medicine, and sometimes surgery are steps to manage it. Eating more fiber, drinking plenty of water, and avoiding certain foods can help. Antibiotics, anti-inflammatory drugs, and pain relievers also play a big role in controlling symptoms.
In serious cases, surgery might be needed. This can change a person’s life for the better. But, managing pain and stress is also important for daily life and happiness.
It’s crucial to work with doctors, like gastroenterologists and surgeons, to manage chronic diverticulitis. Regular visits and personalized plans can help you deal with this condition. This way, you can keep your quality of life as good as possible.
“Managing chronic diverticulitis requires a multifaceted approach, but with the right care and lifestyle modifications, individuals can regain control of their health and find ways to thrive despite the challenges.”
| Symptom | Prevalence |
|---|---|
| Tenderness in the lower abdomen | Common |
| Bloating or gas | Frequent |
| Fever and chills | Occasional |
| Nausea and vomiting | Occasional |
Conclusion
Diverticulitis is a complex digestive condition that can lead to back pain and other symptoms. Understanding its causes, symptoms, and complications helps us seek timely medical care. This knowledge is crucial for managing the condition effectively.
Diverticulitis happens when the pouches in the colon get inflamed. This often causes abdominal pain that can spread to the lower back. While it can be a recurring issue, there are treatments and lifestyle changes that can help manage it.
Working closely with healthcare providers is key. Together, we can find the best treatment for our needs. This proactive approach helps prevent and manage diverticulitis, improving our overall well-being.
FAQ
Can diverticulitis cause back pain?
What is diverticulitis?
What are the common symptoms of diverticulitis?
How is diverticulitis diagnosed?
What are the potential complications of diverticulitis?
How is diverticulitis treated?
How does diet affect diverticulitis?
What are the risk factors for developing diverticulitis?
How can people with chronic diverticulitis manage their condition?
Source Links
- Diverticulosis | Diverticulitis | MedlinePlus – https://medlineplus.gov/diverticulosisanddiverticulitis.html
- 4 Signs that You May Have Diverticulitis: Colon and Rectal Surgeons of Greater Hartford: Colon and Rectal Surgeons – https://www.crsgh.com/blog/4-signs-that-you-may-have-diverticulitis
- Diverticulitis: What It Is, Symptoms, Causes & Treatment Options – https://www.hoag.org/specialties-services/digestive-health/diseases-conditions/diverticulitis-treatment/
- Diverticulitis and Diverticulosis – https://www.uchealth.org/diseases-conditions/diverticulitis-and-diverticulosis/
- Can Diverticulitis Pain Radiate to Your Back? – https://www.verywellhealth.com/diverticulitis-symptoms-back-pain-7483298
- Can Diverticulitis Cause Back Pain? All You Need to Know – https://www.pain-spine.com/2023/10/20/does-diverticulitis-lead-to-back-pain/
- The Symptoms of Diverticulitis – https://www.webmd.com/digestive-disorders/understanding-diverticulitis-symptoms
- Diverticular Disease Expanded Version | ASCRS – https://fascrs.org/patients/diseases-and-conditions/a-z/diverticular-disease-expanded-version
- Diverticulitis and Back Pain Symptoms – Calming Blends – https://calmingblends.com/diverticulitis-and-back-pain-symptoms/
- A Diverticular ‘Pain in the Bottom’ – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1964623/
- Diverticulitis – https://my.clevelandclinic.org/health/diseases/10352-diverticulitis
- Diverticulitis – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/diverticulitis/symptoms-causes/syc-20371758
- Diverticulitis – Diagnosis and treatment – https://www.mayoclinic.org/diseases-conditions/diverticulitis/diagnosis-treatment/drc-20371764
- Patient education: Diverticular disease (Beyond the Basics) – https://www.uptodate.com/contents/diverticular-disease-beyond-the-basics/print
- Diagnosis and Management of Acute Diverticulitis – https://www.aafp.org/pubs/afp/issues/2013/0501/p612.html
- Living with Diverticulitis: The Link Between Back Pain and Diverticulitis – https://www.kaly.com/blog/back-pain-and-diverticulitis/
- Diverticulitis and Back Pain: Causes, Symptoms, and Solutions | Evinature – https://evinature.com/blog/health/understanding-the-connection-between-diverticulitis-and-back-pain/
- Diverticulitis diet – https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/diverticulitis-diet/art-20048499
- Foods for Diverticulosis and Diverticulitis – https://www.hopkinsmedicine.org/health/wellness-and-prevention/foods-for-diverticulosis-and-diverticulitis
- Diverticular disease and diverticulitis symptoms and treatments – https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/diverticular-disease-and-diverticulitis/
- The Basics of Diverticulitis – https://www.webmd.com/digestive-disorders/understanding-diverticulitis-basics
- What Is Diverticulitis? Symptoms, Causes, Diagnosis, Treatment, and Prevention – https://www.everydayhealth.com/diverticulitis/guide/
- Diverticulitis – https://www.mountsinai.org/health-library/diseases-conditions/diverticulitis
- Living with diverticulitis: Get the full scope of symptoms, treatment, and prevention | Digestive | UT Southwestern Medical Center – https://utswmed.org/medblog/diverticulitis-symptoms-treatment/
- Diverticular disease and diverticulitis – https://www.nhs.uk/conditions/diverticular-disease-and-diverticulitis/
- Acute diverticulitis masquerading as unilateral sciatica-like symptoms – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7599022/
- Diverticulitis: Causes, symptoms, and treatments – https://www.medicalnewstoday.com/articles/152995
- Diverticulitis: a comprehensive review with usual and unusual complications – Insights into Imaging – https://insightsimaging.springeropen.com/articles/10.1007/s13244-016-0532-3








