As I sit in the dentist’s chair, the sound of the drill and the smell of disinfectant fill the air. I think about the invisible world in my mouth – the microorganisms that live there. These oral bacteria, both good and bad, are key to my dental health and overall well-being.
Our mouths are full of a complex mix of microbes. These tiny creatures work non-stop, affecting our oral and overall health. They keep a balance that, if upset, can cause many problems. This includes cavities, gum disease, and even serious health issues.
Key Takeaways
- Oral bacteria play a crucial role in dental health and overall well-being.
- A delicate balance of “good” and “bad” bacteria is essential for maintaining a healthy mouth.
- Disruptions to this balance can lead to a variety of dental and systemic health issues.
- Maintaining proper oral hygiene, including daily brushing and flossing, is crucial for controlling the growth of harmful bacteria.
- Emerging research is exploring new ways to target specific bacterial species and protect beneficial microbes in the mouth.
Introduction
Keeping our mouths healthy is key. Our mouths are full of both good and bad bacteria. If we don’t take care of our mouths, the bad bacteria can cause big problems like tooth decay and gum disease.
These problems can spread to other parts of our body and lead to serious health conditions. It’s vital to keep our mouths healthy for our overall health.
Recent studies show that our mouths have a lot of different bacteria, from 20% to 39%. Our genes also play a role in what bacteria live in our mouths. In kids, these bacteria start to form when they are very young.
Studies have found that our mouths have many different communities of bacteria. This shows how important it is to take care of our mouths.
The oral microbiota’s impact on our health is huge. Research shows a strong link between our mouth bacteria and our overall health. This shows how important it is to manage the bacteria in our mouths.
It’s important to understand how our oral health affects our overall health. By taking care of our mouths and managing our oral microbiome, we can stay healthy and avoid many illnesses.
Oral Microbiome: The Good and the Bad
Our mouths are filled with tiny living things called the oral microbiome. Most of these are harmless or even helpful. But a few can cause trouble if they get too many. It’s important to know the balance between good and bad bacteria for good oral health.
There are over 700 types of bacteria in our mouths. Some help with digestion and keep harmful microbes out of our food. But, bacteria like Streptococcus mutans can make tooth enamel dissolve, causing cavities.
Keeping the oral microbiome in balance is crucial. Good bacteria help each other grow and be more beneficial. Yet, too many bad bacteria, like Porphyromonas gingivalis, can lead to bad breath and other problems.
What we eat, how we clean our mouths, and the products we use can change our oral microbiome. Brushing, flossing, and dental check-ups help good bacteria grow and keep bad ones down.
“A balanced microbiome in the mouth is crucial for overall oral health, emphasizing the importance of promoting good bacteria growth and minimizing bad bacteria.”
Learning about the oral microbiome helps us take steps to keep our mouths healthy. This way, our teeth and gums stay in great shape.
Dental Decay: The Role of Streptococcus mutans
Dental decay affects millions of people around the world. At the center of this issue is Streptococcus mutans, a tough bacterium. It’s the main cause of tooth enamel erosion, leading to cavities.
Studies have shown Streptococcus mutans’s key role in tooth decay. Holt et al. in 1994, Lamont et al. in 1991, and Zero in 2004 found strong evidence of this. Desoet et al. in 1990 and Mayooran et al. in 2000 looked at how it affects children’s teeth in various countries.
The Culprit Behind Tooth Erosion
Streptococcus mutans thrives in our mouths. It can make and store polysaccharides, as seen by Toda et al. in 1987 and Wiater et al. in 1999. This lets it keep making acid, eating away at tooth enamel.
This bacterium also forms dental plaque, a protective shield. This makes it hard to fight off, as shown by Phan and Marquis in 2006. The plaque helps keep the bacteria safe.
To fight dental decay, we need to do many things. This includes good oral hygiene at home and seeing a dentist. Using xylitol, as found by Peldyak and Mäkinen in 2002, and antimicrobial agents like triclosan, as seen by van Loveren et al. in 2000 and Garcia-Godoy et al. in 1990, can help.
Periodontal Disease: A Mixed Bacterial Infection
Periodontal disease, also known as gum disease, is a serious issue. It happens when the gums pull away from the teeth because of an inflammatory reaction to plaque bacteria. This condition is often a mix of anaerobic bacteria, like Treponema denticola and Porphyromonas gingivalis.
These anaerobic bacteria make compounds that cause inflammation in the gums. This inflammation can lead to the loss of periodontal tissue. This can cause teeth to become loose or even fall out.
Periodontal disease is a big deal because it affects more than just your mouth’s health. It can also lead to health problems like type 1 diabetes and heart disease.
| Bacterial Species | Role in Periodontal Disease |
|---|---|
| Treponema denticola | Anaerobic bacterium that contributes to the mixed bacterial infection in periodontal disease |
| Porphyromonas gingivalis | Anaerobic bacterium that also plays a role in the mixed bacterial infection associated with periodontal disease |
To fight and manage periodontal disease, keeping your mouth clean is key. Brushing, flossing, and regular dental check-ups are essential. Sometimes, doctors may also prescribe medicines like metronidazole or doxycycline to tackle the bacteria.
How oral bacteria affect dental health
Our bodies are full of tiny living things, especially in our mouths and guts. In fact, we have about 39 trillion of these tiny creatures, which include bacteria, viruses, and fungi. This is more than the 30 trillion human cells in our bodies.
Having trillions of bacteria in our mouths might sound scary, but it’s actually important. Good bacteria keep our mouths healthy, while bad bacteria can cause tooth decay and gum disease.
The Impact of Oral Bacteria
When the balance of bacteria in our mouths gets off, it can cause big problems. Studies show that bacteria move from our mouths to our guts more often than we thought. This means our mouth bacteria can affect our gut health a lot.
Too many bad bacteria can lead to serious health issues, like Alzheimer’s disease, diabetes, and heart disease. Some gut bacteria can even make our teeth unstable, similar to gum disease.
Maintaining Oral Bacterial Balance
Keeping the right balance of bacteria in our mouths is key for our health. If the balance is off, we can get gum inflammation, tooth decay, and bad breath. Bad bacteria in our mouths can also cause infections and lung diseases.
Probiotics can help fix the balance of good and bad bacteria in our mouths. By understanding how oral bacteria work and keeping them in balance, we can keep our teeth and overall health strong.
| Beneficial Oral Bacteria | Harmful Oral Bacteria |
|---|---|
|
|
“The balance of beneficial and harmful bacteria in the oral microbiome is crucial for maintaining a healthy mouth and preventing dental problems.”
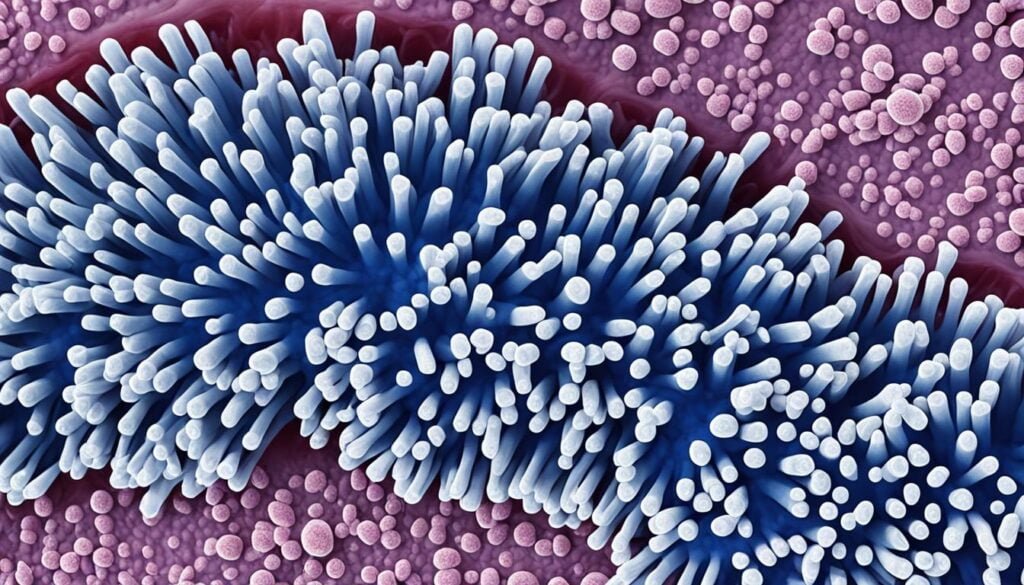
The Plaque Matrix: A Protective Shield for Bacteria
Dental plaque is a sticky film that forms on our teeth. It’s filled with many kinds of bacteria. These bacteria create a slimy matrix that protects them from being washed away.
This matrix makes plaque tough to clean, letting the bacteria grow and potentially harm our teeth and gums.
Understanding the Bacterial Community
Our mouths are home to hundreds of different bacteria. A study in 2012 found a balance of these microorganisms in our mouths. By 2018, scientists had analyzed the oral microbiota, showing a wide variety of bacteria present.
The plaque matrix is key in this bacterial community. It helps maintain a balance in the mouth, showing how important it is for the bacteria.
As plaque matures, it becomes harder to remove because of its changing composition. Saliva’s proteins and minerals help bacteria stick to teeth, making plaque worse. When bacteria break down sugars, they produce acid, which helps plaque grow and spread.
If plaque is not treated, it can cause many oral health problems. These include tooth decay, gum disease, and even heart disease and diabetes. Regular dental cleanings can remove the biofilm before it turns into hard plaque, preventing serious damage.
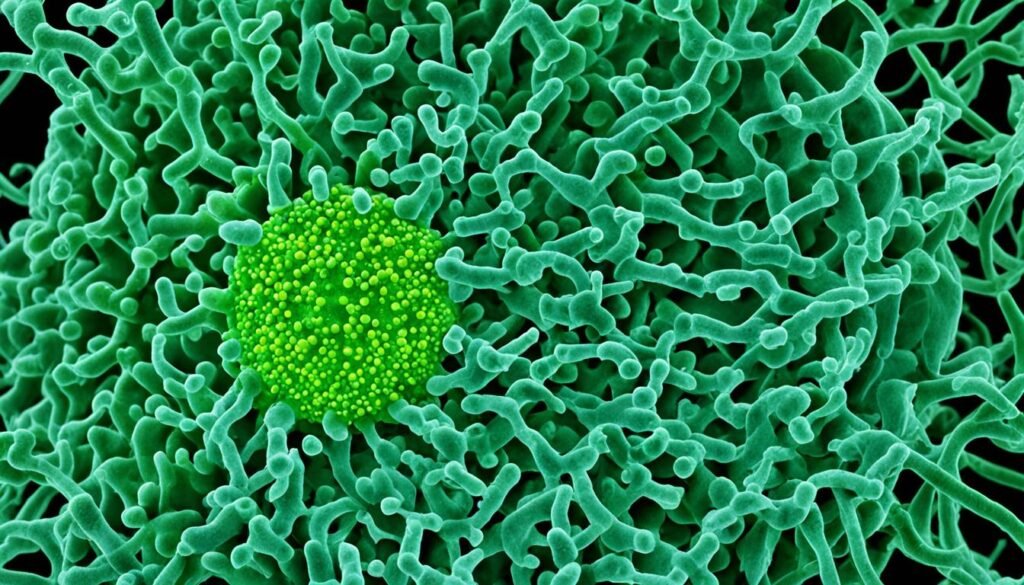
Early Childhood Tooth Decay: A Bacterial and Fungal Partnership
Early childhood tooth decay affects about 23% of kids aged 1 to 5 in the U.S. It’s caused by a partnership between bacteria and fungus in plaque on kids’ teeth. This partnership leads to fast tooth decay.
The fungus grows on the acid made by bacteria. It helps the bacteria form a strong, protective layer. This layer lets the bacteria make more acid, which worsens tooth decay. This creates a cycle that can cause severe tooth decay if not stopped.
A study looked at the mouths of kids with severe tooth decay and those without. It found big differences in the fungi in their mouths. This shows that the interaction between fungus and bacteria is key to tooth decay in young kids.
| Oral Microbiome Findings | SECC | ECC | Caries-Free |
|---|---|---|---|
| Dominant Bacterial Genera | Haemophilus 2, Bergeyella, Gemella, Streptococcus | Streptococcus, Haemophilus (Haemophilus 1 and 2), Neisseria, Gemella, Porphyromonas | More diverse community |
| Salivary Fungal Community | Significant alterations | Significant alterations | No significant changes |
| Bacterial-Fungal Interactions | 5 fungal types impacted bacterial structure | 5 fungal types impacted bacterial structure | Minimal impact |
This research shows how important it is to understand how bacteria and fungi work together in tooth decay. By focusing on these interactions, we can fight this condition and keep kids’ smiles healthy.
Saliva: Nature’s Defense Against Oral Bacteria
Saliva is a key fluid in our mouth that keeps us healthy. It washes away food bits and keeps the mouth’s pH balanced. It also has compounds that stop harmful bacteria from growing.
Without enough saliva, harmful bacteria can grow too much. This can lead to tooth decay and other mouth problems. Saliva acts as a vital defense against oral bacteria, keeping us safe.
Salivary antimicrobial peptides, like cathelicidins, help our oral health. They fight off Candida albicans, a common mouth fungus. Histatins in saliva help heal wounds too.
“Saliva functions as a crucial antimicrobial defense system for the oral cavity.” – van ‘t Hof, Veerman, Nieuw Amerongen, and Ligtenberg (2014)
Changes in saliva can show health issues. For example, salivary calprotectin levels are high in some mouth infections or Sjögren’s syndrome. But they’re low in people with HIV.
Knowing how saliva fights oral bacteria shows why good mouth care is important. Keeping our saliva and oral balance helps us smile happily and healthily.
Oral Hygiene: The Frontline Defense
Good oral hygiene is key to fighting off harmful oral bacteria. Brushing, flossing, and regular dental check-ups are vital. They help stop dental decay, gum disease, and other oral health issues.
Brushing, Flossing, and Professional Cleanings
Brush your teeth twice a day, once when you wake up and once before you go to bed. This removes plaque and food bits. Flossing every day is also crucial. It gets rid of particles your toothbrush misses, stopping plaque from building up.
Don’t forget about regular dental cleanings. A dentist or dental hygienist can remove plaque and tartar that’s hard to get rid of at home. This ensures a deep clean and keeps your mouth healthy.
| Oral Hygiene Practice | Benefit |
|---|---|
| Brushing | Removes plaque and food debris |
| Flossing | Reaches areas that brushing can’t access, preventing plaque buildup |
| Professional Cleanings | Removes hardened plaque and tartar that are difficult to remove at home |
Adding these key oral hygiene steps to your daily routine helps fight off bad bacteria. This keeps your smile healthy and bright.
“Proper oral hygiene is the key to preventing dental problems and maintaining a healthy mouth.”
Fluoride: A Powerful Ally Against Dental Decay
Fluoride is a key mineral that helps keep our teeth healthy. It makes tooth enamel stronger and helps teeth heal from decay. This is why fluoride is added to our water, toothpaste, and some treatments. It has greatly reduced cavities in many countries.
About 62% of people in the U.S. get enough fluoride from their water. 43 out of 50 large U.S. cities add fluoride to their water. This has been a big help in fighting cavities, especially in kids under 6 who are still getting their permanent teeth.
But not all water is the same. Some systems, like steam distillation, can remove 100% of fluoride. Reverse osmosis takes out 65% to 95%, and some filters remove over 80%. So, knowing what’s in your water is important.
Fluoride toothpaste is also a great tool against cavities. It helps prevent decay in growing teeth. In the U.S., toothpaste usually has 1,000 to 1,100 parts per million (ppm) of fluoride. Brushing with it twice a day can cut cavity risk by 14%.
But we must use fluoride carefully. Too much can cause fluorosis, which can harm tooth enamel in kids. Dentists use stronger fluoride treatments for those at high risk of cavities.
In summary, fluoride is a big help in fighting cavities. Its use in water, toothpaste, and treatments has made oral health better around the world. By knowing how to use fluoride right, we can keep our teeth strong and healthy for life.
| Fluoride Removal Method | Percentage of Fluoride Removed |
|---|---|
| Steam Distillation | 100% |
| Reverse Osmosis | 65% – 95% |
| Activated Carbon Filters with Activated Alumina | over 80% |
Antimicrobial Therapies: The Future of Oral Health
Researchers are looking into new ways to fight oral health problems. These new methods aim to stop and treat dental issues better. This could lead to a brighter future for our oral health.
Targeting Specific Bacterial Species
Nanoparticles are being studied to target bad bacteria in dental plaque. These tiny particles can get through the plaque’s protective layer. They then attack and stop bacteria like Streptococcus mutans without harming good bacteria.
This could help fight antibiotic resistance in dentistry. Antibiotics have made some bacteria resistant, making infections harder to treat. Antimicrobial therapies that target only the bad bacteria could be a game-changer.
These new ways to manage oral health could change the game. They could improve not just our mouths but our overall health too. The link between oral health and other diseases means these therapies could make a big difference.
As research goes on, the role of nanoparticles and other new treatments in oral health is becoming clear. These technologies could change how we keep our mouths healthy. With them, antimicrobial therapies could be key to a healthy mouth.
“The future of oral health lies in our ability to understand and harness the complex dynamics of the oral microbiome. Targeted antimicrobial therapies offer a promising avenue to address the growing challenges in dental care and promote long-term oral well-being.”
Systemic Health Implications
Your mouth’s health greatly affects your overall well-being. Oral infections and inflammation are linked to many health issues, like heart disease, stroke, diabetes, and pregnancy complications. Keeping your mouth clean and treating any health problems is key. It helps protect your general health and stops harmful bacteria from spreading.
About up to 50% of adults may have periodontal disease, a serious infection. This can lead to health problems all over the body. Also, nearly half of Americans have a risk factor for heart disease, like diabetes, obesity, or smoking. These can get worse with poor oral health.
There’s a strong connection between oral bacteria and systemic health effects. Studies show that certain oral bacteria can cause cardiovascular disease, chronic kidney disease, diabetes, and some cancers. These microbes in our mouths can also weaken our immune system and increase inflammation, affecting our systemic health.
To keep your body healthy, focus on oral hygiene and fix any health problems quickly. Regular dental visits, brushing, flossing, and fluoride use can help. They keep your mouth healthy and stop harmful infections from spreading.
“The health of your mouth is closely tied to the health of your body as a whole. Neglecting your oral hygiene can have serious consequences for your overall well-being.”
Conclusion
Thinking about oral health and the role of oral bacteria shows how our mouth affects our overall health. The balance of oral bacteria is key to keeping our mouth healthy. It also helps protect us from many health problems.
Studies reveal a deep link between oral bacteria and various health issues. These include cancer, neurodegenerative diseases, bone health, and cognitive function. The connection between the gut and oral microbiome highlights the need for good oral hygiene.
By brushing, flossing, and visiting the dentist regularly, we can keep our oral microbiome in balance. This protects our teeth and gums. New advances in dentistry and the use of the oral microbiome help prevent and treat dental issues. They improve our health and quality of life.
FAQ
How do oral bacteria affect dental health?
What is the oral microbiome and how does it impact dental health?
What is the role of Streptococcus mutans in dental decay?
How do anaerobic bacteria contribute to periodontal disease?
What is the role of saliva in maintaining oral health?
How can good oral hygiene help prevent dental problems?
How does fluoride help protect against dental decay?
What are some new antimicrobial therapies for oral health?
How can poor oral health affect overall health?
Source Links
- https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475 – Oral health: A window to your overall health
- https://newsinhealth.nih.gov/2019/05/mouth-microbes – Mouth Microbes
- https://www.choice-dental.com.au/how-oral-bacteria-can-affect-the-rest-of-your-body/ – How Oral Bacteria Can Affect the Rest of Your Body
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6503789/ – Oral microbiome: Unveiling the fundamentals
- https://clinmedjournals.org/articles/ijodh/international-journal-of-oral-and-dental-health-ijodh-7-127.php?jid=ijodh – Oral Biofilm and Its Impact on Oral Health, Psychological and Social Interaction
- https://www.listerine.com/fresh-breath/good-vs-bad-oral-microbiome-bacteria – The Oral Microbiome: Good vs. Bad Bacteria in Your Mouth | LISTERINE®
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10690560/ – Mouthwash Effects on the Oral Microbiome: Are They Good, Bad, or Balanced?
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257652/ – Streptococcus mutans, Caries and Simulation Models
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC373078/ – Role of Streptococcus mutans in human dental decay.
- https://www.ncbi.nlm.nih.gov/books/NBK8259/ – Microbiology of Dental Decay and Periodontal Disease – Medical Microbiology
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC88948/ – Systemic Diseases Caused by Oral Infection
- https://southdakota.deltadental.com/blog/connection-between-oral-health-and-gut-health/ – The connection between oral health and gut health
- https://ahoa.es/en/bacteria-affect-our-dental-health/ – How do bacteria affect our dental health?
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6646062/ – The structure of dental plaque microbial communities in the transition from health to dental caries and periodontal disease
- https://arlingtonsmilesdentalstudio.com/formation-of-dental-plaque-explained/ – Formation of Dental Plaque Explained | Arlington Smiles Dental Studio
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9413593/ – The dental plaque biofilm matrix
- https://www.nature.com/articles/s41598-024-59126-z – Early life factors and oral microbial signatures define the risk of caries in a Swedish cohort of preschool children – Scientific Reports
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4114182/ – Fungal-bacterial interactions and their relevance to oral health: linking the clinic and the bench
- https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.845738/full – Frontiers | The Crosstalk Between Saliva Bacteria and Fungi in Early Childhood Caries
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6855406/ – The power of saliva: Antimicrobial and beyond
- https://www.nature.com/articles/sj.bdj.2016.865 – The oral microbiome – an update for oral healthcare professionals – British Dental Journal
- https://www.nduclinic.com/blog/2024/3/4/jadn6nbbqttdixttvrmdi2co3u5wyj – Mouth Matters: The Link Between Oral Health and Your Well-Being — ndu Clinic
- https://www.integrity-dental-inc.com/dental-services/blog/does-oral-health-affect-overall-health – Does oral health affect overall health?
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9866409/ – An Outlook on Dental Practices to Avoid the Oral Transmission of COVID-19
- https://www.webmd.com/oral-health/fluoride-treatment – What is Flouride?
- https://www.ncbi.nlm.nih.gov/books/NBK587342/ – The Role of Fluoride on Caries Prevention – StatPearls
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9778414/ – Managing Oral Health in the Context of Antimicrobial Resistance
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7013294/ – Application of Antibiotics/Antimicrobial Agents on Dental Caries
- https://www.ada.org/resources/ada-library/oral-health-topics/oral-systemic-health – Oral Systemic Health
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9678577/ – The systemic oral health connection: Biofilms
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9405223/ – Oral Microbiota, Its Equilibrium and Implications in the Pathophysiology of Human Diseases: A Systematic Review
- https://mouth.co.uk/how-your-oral-hygiene-affects-your-overall-health/ – How your oral hygiene affects your overall health – Mouth Dental