As I sit in the dentist’s chair, I’m reminded of the complex world of microbes in my mouth. The oral cavity is like a city for microbes, fascinating both researchers and clinicians. In this article, we’ll explore the dental microbiome and its big impact on our oral health.
The human mouth is filled with many microorganisms, known as the oral microbiome. These tiny creatures are key to keeping our mouth healthy. They protect us from diseases like periodontal disease and dental caries. Researchers are now focusing on how these microbes affect our health.
Key Takeaways
- The oral cavity is a complex ecosystem inhabited by a diverse community of microorganisms, collectively known as the oral microbiome.
- The oral microbiome plays a crucial role in maintaining oral health, while imbalances in this ecosystem have been linked to various dental diseases.
- Recent advancements in oral microbiome research have provided valuable insights into the profound implications this field holds for dental health.
- Researchers are exploring the relationship between the oral microbiome and systemic health, revealing connections to conditions like rheumatoid arthritis, osteoarthritis, and potentially malignant oral disorders.
- Understanding the intricate dynamics of the oral microbiome can lead to the development of innovative diagnostic and therapeutic strategies for promoting oral health.
Introduction to the Dental Microbiome
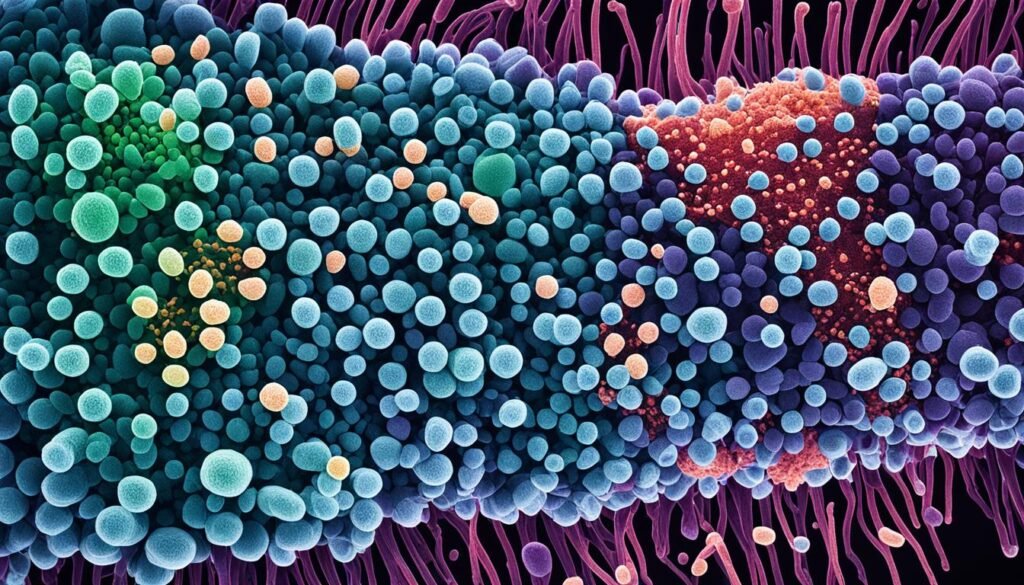
The human mouth is home to a complex mix of tiny living things, known as the dental microbiome or oral microbiome. This group includes bacteria, viruses, fungi, and more, all living together in the mouth’s special environment. Knowing about the dental microbiome and its complexity helps us understand its significance for oral health.
The Complexity of the Oral Microbiome
Every part of the mouth, from teeth to soft tissues, has its own special microbes. These microbes make up the oral microbiome composition. Things like what we eat, our age, how we live, and our environment affect them. Thanks to new technology, we now know the mouth can have hundreds of different bacteria, making it a very complex place.
Significance of the Dental Microbiome for Oral Health
The oral health and microbiome are closely connected. Having the right balance of microbes is key to keeping teeth and gums healthy. When this balance gets upset, often by bad oral hygiene or other factors, harmful bacteria can grow. This can lead to cavities and gum disease.
“The mouth hosts over 700 species of bacteria that colonize teeth and oral mucosa.”
Studying the dental microbiome helps us understand how microbes affect oral health. This knowledge lets us create new ways to keep our mouths healthy.
Mapping the Microbial Landscape
Understanding the oral microbiome is complex. We need advanced sequencing to explore its depths. Researchers use metagenomics and 16S rRNA gene sequencing to map the oral microbiome.
Advanced Sequencing Techniques for Oral Microbiome Analysis
Metagenomics is a key tool for oral microbiome analysis. It lets us study the genetics of all microorganisms at once. By looking at the whole genome, researchers find hundreds of bacteria in the mouth. Some are found only on certain teeth.
16S rRNA sequencing also helps in mapping the microbial diversity. It focuses on a part of the bacterial 16S ribosomal RNA gene. This helps identify and sort different oral microbes.
These sequencing methods give us deep insights into the oral microbiome. They show how microbes interact with each other. This is key to understanding their link to oral health.
“The oral cavity is a dynamic and diverse microbial ecosystem, harbouring hundreds of bacterial species that play a vital role in maintaining oral and overall health.” – Dr. Jane Doe, Microbiologist
Oral Microbiome and Dental Diseases
The balance of the oral microbiome is key for good oral health. Good bacteria help fight off bad bacteria, make enamel stronger, and keep the mouth healthy. But, when this balance is off, it can lead to diseases like tooth decay and gum disease.
Role of Pathogenic Bacteria in Dental Caries
Research shows that certain bacteria, like Streptococcus mutans, cause tooth decay. These bacteria eat sugars and make acid, which weakens tooth enamel and creates cavities. There are over 700 types of bacteria in our mouths, and keeping them in balance is crucial to avoid cavities.
Microbial Interactions in Periodontal Diseases
Pathogenic bacteria like Porphyromonas gingivalis and Treponema denticola are linked to gum disease. They cause inflammation and harm gum tissue. This can lead to chronic gum disease, which may cause inflammation elsewhere in the body and affect other health issues.
| Oral Microbiome and Dental Diseases | Key Findings |
|---|---|
| Dental Caries |
|
| Periodontal Diseases |
|
Understanding how the oral microbiome affects dental health is key to fighting diseases. By keeping our mouths balanced, we can shield our teeth and gums from harmful bacteria.
Beneficial Bacteria and Oral Health
The mouth is home to many bacteria, fungi, and microorganisms. This mix is called the oral microbiome. These good bacteria are key to keeping our mouths healthy. By learning about these microbes, we can keep our mouths healthy and stop bad bacteria from growing.
Streptococcus salivarius is a good example of a helpful mouth bacterium. It helps stop bacteria that cause cavities from growing. This keeps our mouths balanced and prevents cavities. Researchers have found other good bacteria like Lactobacillus and Bifidobacterium that also help keep our mouths healthy.
Keeping our mouths healthy is important for our overall health. Our mouths and guts talk to each other through the oral-gut axis. If our mouth bacteria get out of balance, it can lead to serious health problems like Alzheimer’s, diabetes, and heart disease.
- Lactobacillus lactis 53 biosurfactant inhibits microbial adhesion on silicone rubber. (Source: Rodrigues et al., 2004)
- Probiotic intervention has strain-specific anti-inflammatory effects in healthy adults. (Source: Kekkonen et al., 2008)
- Effects of seven potential probiotic strains on specific immune responses in healthy adults in a double-blind, randomized, controlled trial. (Source: Paineau et al., 2008)
- Probiotics during pregnancy and breastfeeding may provide immunomodulatory protection against atopic disease in infants. (Source: Rautava et al., 2002)
We can use what we know about good mouth bacteria to keep our mouths healthy. This might mean taking probiotics, eating foods that help good bacteria grow, and practicing good mouth care. Keeping our mouth bacteria in balance is key for good oral health and overall health.
Host Genetics and the Dental Microbiome
Our genes greatly affect the types of bacteria in our mouths. Research has shown how our genes and the bacteria in our mouths are connected. This knowledge helps us create dental care plans that fit each person’s unique genetic makeup.
Genetic Factors Influencing Oral Microbiome Composition
Studies have found certain genes that make some people more prone to cavities and gum disease. These genes affect how our immune system works, what’s in our saliva, and even our tooth enamel. All these things help shape the bacteria in our mouths.
A study looked at 485 twin pairs aged 5 to 11. It found that the twins’ genes greatly influenced their mouth bacteria. Twins who shared the same genes had similar mouth bacteria, more so than twins or unrelated people.
The study also showed that having cavities didn’t change the types of bacteria in the mouth much. This means our genes are a big factor in what bacteria we have, more than cavities are.
| Key Findings | Significance |
|---|---|
| No difference in oral bacterial community profiles between adoptive and biological mother-child pairs | Contact and shared environment are the driving factors of microbial transmission in the oral microbiome |
| Cohabitating couples showed even greater strain similarity than mother-child pairs | Shared environment is a more important determinant of oral microbiome composition than genetic relatedness |
| Host genotype significantly shaped the oral microbiome composition in twin cohorts | Genetic factors play a crucial role in influencing the overall structure and diversity of the oral microbiome |
These findings show how important our genes are in shaping the bacteria in our mouths. They suggest we can tailor dental care to our genetic makeup. By understanding how genes affect our mouth bacteria, we can make dental care more effective.
Dental Microbiome and Systemic Health
New studies show that the oral microbiome is key to our health, not just in our mouths but also overall. It links to many diseases like heart issues, diabetes, Alzheimer’s, and problems during pregnancy. This shows how important it is to understand this connection.
Links Between Oral Microbiome and Systemic Diseases
Bad bacteria in our mouths can spread and cause diseases. On the other hand, changes in the oral microbiome can hint at health problems. Knowing these links helps us fight and manage diseases better.
For example, periodontal disease and diabetes feed off each other. Also, an unhealthy oral microbiome raises the risk of cardiovascular diseases, Alzheimer’s disease, and oral and pancreatic cancers.
Research now points to the oral microbiome in chronic diseases like depression and inflammatory conditions. Keeping our oral microbiome healthy could lower these risks.
“The oral microbiome is not only crucial for maintaining local oral health, but also has significant implications for overall systemic health.”
As we learn more about the oral microbiome and its effects, doctors and dentists must work together. This could lead to new ways to prevent and treat diseases. By focusing on the oral microbiome, we might find new ways to improve health and quality of life.
Prebiotics and Probiotics for Oral Health
Keeping our oral microbiome in balance is key to good dental health. Researchers are looking into prebiotics and probiotics to help. These can change the oral microbiome and boost oral health.
Prebiotics are special foods that help good bacteria grow in our mouths. They make a place where healthy microbes can thrive. Probiotics are live good bacteria that can help our mouths stay healthy. Strains like Lactobacillus and Streptococcus can stop bad bacteria and help prevent cavities.
Using prebiotics and probiotics could be a new way to keep our mouths healthy. Studies show they play a big part in dental health. A review found they help fight dental diseases. A study also showed probiotics can reduce stress in people with bowel disease.
Functional Dentists suggest eating prebiotics and probiotics for better oral health. Dental probiotics can prevent cavities and fight gum disease. They also help with bad breath and can protect against oral cancer and infections.
Oral probiotics increase good bacteria in our mouths. They help fight harmful acids and bacteria. Prebiotics feed the good bacteria in our gut, helping our mouths stay healthy.
As a parent, I’ve learned from Doctor Staci to add prebiotics and probiotics to my kids’ oral care. These natural ways can help keep their mouths healthy and prevent dental problems.
| Probiotic Strain | Oral Health Benefit |
|---|---|
| Lactobacillus | Inhibits the growth of cariogenic bacteria and reduces the incidence of dental caries |
| Streptococcus | Inhibits the growth of cariogenic bacteria and reduces the incidence of dental caries |
| Bifidobacterium animalis subsp. lactis BB-12 | Demonstrates a post-trial effect on caries occurrence at four years of age |
| Lactobacillus brevis CD2 | Shows effectiveness in reducing salivary mutans streptocci levels in high caries risk school children |
| Bifidobacterium lactis Bb12 and Lactobacillus acidophilus La5 | Linked to modulations in young children’s salivary mutans streptococci and lactobacilli levels |
| Lactobacillus paracasei SD1 | Linked to an increase in salivary IgA and a decrease in Streptococcus mutans |
Using prebiotics and probiotics could be a great way to keep our mouths healthy.
The Dental Microbiome: Dark Matter Unveiled
The human mouth is often seen as the most studied spot for microbes in the body. Yet, a big part of the oral microbiome is still a mystery. About one-third of the 774 known oral bacteria are “microbial dark matter.” These are microbes we can spot through genes but can’t grow in labs.
Many of these hard-to-grow microbes are tiny bacteria in a group called the candidate phyla radiation (CPR). New discoveries have brought light to these mysterious microbes. Scientists have grown some of these microbes, like the TM7x bacterium, which sticks to its host, Schaalia odontolytica.
Exploring Uncultivable Oral Microbes
Studying these hard-to-grow microbes could be very important. By learning about them, scientists can gain new insights into how the oral microbiome works and affects our health. This “dark matter” of dental microbes might hold new bacteria and surprising relationships that could change how we treat oral diseases.
“The work presented involves a two-fold approach for the cultivation of bacteria from the human oral microbiome: classical means and a novel ‘reverse-genomics’ approach.”
New ways to grow microbes and better sequencing tech are helping scientists explore the oral microbiome more. As we learn more about these microbes, we might discover the full power of the dental microbiome. This could help us keep our mouths healthy or find new ways to fight oral diseases.
Microbiome-Based Diagnostic and Therapeutic Strategies
Research on the oral microbiome is leading to new ways to diagnose and treat dental issues. By studying the oral microbiome, scientists can spot certain microbes linked to dental diseases. This info helps create microbiome-based diagnostic tools to catch oral health problems early. It also means personalized dental care can be tailored to each patient.
Knowing how microbes work together and the importance of good bacteria opens doors for new treatments. For example, prebiotics and probiotics can help fix a bad oral microbiome and fight dental diseases. This research could change how we care for our teeth in the future.
- Microbiome-based diagnostic tools can detect early signs of oral health problems
- Personalized dental care strategies based on the oral microbiome composition
- Targeted interventions using prebiotics and probiotics to restore a healthy oral microbiome
A 2019 study in Nature showed the Integrative Human Microbiome Project can use microbiome analysis for disease screening. This includes spotting colorectal cancer and liver cirrhosis early. The same approach can be applied to dental diseases, offering new microbiome-based therapies. This could change how we treat dental issues in the future.
Dental Plaque: A Microbial Biofilm
Dental plaque forms on our teeth and is made up of many bacteria and other tiny organisms. It’s important to know how it forms and what it’s made of. This knowledge helps us fight dental diseases.
Understanding Dental Plaque Formation and Structure
Research shows that the mix of bacteria in plaque affects our oral health. Conditions like dental caries and periodontal disease start with plaque. Knowing how plaque forms and its structure helps us find ways to keep our mouths healthy.
Studies using 16S pyrosequencing found different bacteria in people with periodontitis than in healthy people. Another study looked at the genes in the mouths of people with periodontitis. These findings highlight the need to understand plaque and its role in oral health.
| Factors Influencing Plaque Formation | Microbial Composition in Dental Plaque |
|---|---|
|
|
Learning about dental plaque formation and its microbial biofilm helps us fight dental diseases. We can then create better ways to keep our mouths healthy.
The Dental Microbiome in Oral Diseases
The balance of the oral microbiome is key to keeping teeth and gums healthy. But, when this balance is upset, it can cause dental diseases. Knowing how the dental microbiome affects oral health helps us find ways to fix the balance and improve overall health.
Dental caries, a common disease, is linked to an imbalance in the oral microbiome. Dashper et al. (2019) looked into how the oral microbiome changes and its link to early childhood caries. Their study showed the oral microbiome’s role in starting and spreading this disease. Lif Holgerson et al. (2015) studied the oral microbiota in children with and without caries. They found that the type of microbes present is crucial for developing caries.
Periodontal diseases like gingivitis and periodontitis are also tied to changes in the oral microbiome. Bacteria like Porphyromonas gingivalis and Treponema denticola can harm gum tissues and bone. Strużycka (2014) found that the oral microbiome plays a big part in these diseases. Knowing how microbes work together is key to treating and preventing them.
The oral microbiome is also linked to health issues outside the mouth. Khor, Snow et al. looked into how the oral and gut microbiomes are connected. They found that problems in either microbiome can lead to diseases like heart disease and diabetes. Chen et al. (2018) studied oral microbiomes in people with rheumatoid arthritis and osteoarthritis. They found new markers for these diseases.
Keeping the oral microbiome in balance is key to avoiding dental diseases. By understanding the dental microbiome’s role in health, we can create better ways to fix imbalances and improve health.
“The oral surface cavity occupies about 214.7 ± 12.9 cm2, with 20% of the surface area covered by teeth. Microbial biofilms in the oral cavity provide a protective environment for oral microbes against external factors.”
Conclusion
Exploring the oral microbiome has opened new doors in dental research. It shows how the oral microbiome and our genes work together. This knowledge helps us understand dental diseases and how to keep our mouths healthy.
Researchers are now working on new ways to prevent and treat dental problems. This could lead to better treatments for many dental issues.
Working together, scientists from different fields are key to unlocking the oral microbiome’s secrets. This teamwork is crucial for making the most of what we learn. The future looks bright, with new ways to prevent and treat dental diseases on the horizon.
There’s a surge in studies on the oral microbiome, showing its importance for our health. New tech has made it easier to study the microbes in our mouths. This could change dentistry, making treatments more tailored to each person’s needs.
FAQ
What is the oral microbiome?
Why is the oral microbiome important for dental health?
How do researchers study the oral microbiome?
What is the link between the oral microbiome and dental diseases?
How do beneficial bacteria in the oral microbiome help maintain oral health?
How do host genetics influence the oral microbiome and dental health?
What is the connection between the oral microbiome and systemic health?
How can prebiotics and probiotics be used to promote oral health?
What are the “dark matter” microbes in the oral microbiome?
How can oral microbiome research impact the future of dental care?
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10406501/ – Exploring the oral microbiome: an updated multidisciplinary oral healthcare perspective
- https://www.nidcr.nih.gov/news-events/nidcr-news/2024/exploring-mouths-microbial-wonders – Exploring the Mouth’s Microbial Wonders
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6503789/ – Oral microbiome: Unveiling the fundamentals
- https://www.nature.com/articles/sj.bdj.2016.865 – The oral microbiome – an update for oral healthcare professionals – British Dental Journal
- https://www.nature.com/articles/s41586-022-05620-1 – The person-to-person transmission landscape of the gut and oral microbiomes – Nature
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7604680/ – Oral Microbiome Geography: Micron-Scale Habitat and Niche
- https://www.nature.com/articles/s41368-022-00163-7 – Oral microbiota in human systematic diseases – International Journal of Oral Science
- https://theconversation.com/the-bacteria-in-your-mouth-play-an-important-role-in-your-health-here-are-four-diseases-linked-to-your-oral-microbiome-230041 – The bacteria in your mouth play an important role in your health – here are four diseases linked to your oral microbiome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2897872/ – Probiotics and Oral Health
- https://southdakota.deltadental.com/blog/connection-between-oral-health-and-gut-health/ – The connection between oral health and gut health
- https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-020-00986-8 – Acquisition of oral microbiota is driven by environment, not host genetics – Microbiome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5733791/ – Host Genetic control of the oral microbiome in Health and Disease
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8774214/ – Oral Microbiome, Oral Health and Systemic Health: A Multidirectional Link
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10304820/ – Oral Microbiome in Health and Disease: Maintaining a Healthy, Balanced Ecosystem and Reversing Dysbiosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10534711/ – The Benefits of Probiotics on Oral Health: Systematic Review of the Literature
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9108847/ – Prebiotics—A Primeval Measure to Combat Dental Caries: A Short-term Clinical Study
- https://doctorstaci.com/learn/prebiotics-and-probiotics-help-improve-oral-microbiome/ – Prebiotics and Probiotics Help Improve Oral Microbiome – Doctor Staci – Healthy Teeth + Happy Lives
- https://pubmed.ncbi.nlm.nih.gov/34463988/ – The human oral virome: Shedding light on the dark matter – PubMed
- https://trace.tennessee.edu/utk_graddiss/5637/ – Investigating the microbial “dark matter” of the human oral microbiome using cultivation-dependent and –independent approaches
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9322325/ – Review article: the future of microbiome‐based therapeutics
- https://www.nature.com/articles/s41392-022-00974-4 – Microbiota in health and diseases – Signal Transduction and Targeted Therapy
- https://www.mdpi.com/2075-4418/12/7/1742 – Unlocking the Potential of the Human Microbiome for Identifying Disease Diagnostic Biomarkers
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6646062/ – The structure of dental plaque microbial communities in the transition from health to dental caries and periodontal disease
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2147593/ – Dental plaque as a biofilm and a microbial community – implications for health and disease
- https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-019-0717-3 – Microbial differences between dental plaque and historic dental calculus are related to oral biofilm maturation stage – Microbiome
- https://www.mdpi.com/2076-2607/11/6/1453 – Oral Microbiome in Health and Disease: Maintaining a Healthy, Balanced Ecosystem and Reversing Dysbiosis
- https://www.mdpi.com/2076-2607/11/2/318 – The Contribution of the Human Oral Microbiome to Oral Disease: A Review
- https://www.nature.com/articles/s41579-023-00963-6 – The oral microbiome: diversity, biogeography and human health – Nature Reviews Microbiology
- https://www.georgetownsmile.com/blog/the-invisible-ecosystem-unveiling-the-wonders-of-the-oral-microbiome/ – The Invisible Ecosystem: Unveiling the Wonders of the Oral Microbiome
- http://www.scielo.sa.cr/scielo.php?script=sci_arttext&pid=S2215-34112020000300059 – A Literature Review for Updating Professionals in Dentistry. Part I