As I sat in the dentist’s chair, the gentle hum of the equipment and the familiar scent of antiseptic filled the air. It was then that I realized the true importance of my oral health – not just for my teeth, but for my overall wellbeing. The bacteria living in my mouth, known as the oral microbiome, play a crucial role in maintaining my physical and mental health. They’re not just a bunch of germs, but a complex community that can either support or undermine my health.
In this guide, we’ll dive deep into the world of oral bacteria. We’ll explore the intricate balance of the oral microbiome and how it can impact our lives in ways we never imagined. From understanding the types of beneficial and harmful bacteria to the far-reaching effects they can have on our bodies, this article will equip you with the knowledge to take control of your mouth health and, in turn, your overall health.
Key Takeaways
- The oral microbiome consists of over 700 species of bacteria, along with fungi, viruses, and protozoa, all of which play a crucial role in oral and overall health.
- A healthy oral microbiome helps prevent harmful pathogens, while an imbalance (dysbiosis) can lead to issues like bad breath, tooth decay, and gum disease.
- Chronic inflammation in the mouth can have systemic effects, potentially contributing to conditions like cardiovascular disease, diabetes, and autoimmune disorders.
- Factors like poor oral hygiene, diet, lifestyle choices, and certain medications can contribute to oral dysbiosis.
- Proactive steps, such as maintaining good oral hygiene, visiting the dentist regularly, and seeking personalized guidance, can help restore the balance of the oral microbiome and improve overall wellness.
Introduction to the Oral Microbiome
The human body is filled with tiny living things called the microbiome. This includes the mouth, where a special group of microbes live. They work together in a balance, making up the oral microbiome.
What is a Microbiome?
A microbiome is full of tiny living things that live in a certain place. These can be bacteria, viruses, and fungi. They are key parts of the body’s natural balance.
The Complexity of the Oral Microbiome
Our mouths have a huge variety of microbes, with about 700 types of them. They live on our teeth, gums, tongue, cheeks, and in our saliva. What we eat, how we take care of our mouths, and our health affects them.
| Oral Microbiome Composition | Percentage |
|---|---|
| Bacteria | 97% |
| Archaea | 1% |
| Fungi | 2% |
The oral microbiome is complex and full of life. It’s important to understand it to keep our mouths healthy. This knowledge helps us deal with health issues linked to the balance of our mouth’s microbes.
Beneficial Bacteria in the Mouth
The human mouth is home to a wide variety of bacteria, both good and bad. It’s filled with microbes like bacteria, fungi, and viruses. These play a key role in keeping our mouths healthy when they’re in balance.
Types of Beneficial Oral Bacteria
Beneficial bacteria in the mouth include Streptococcus, Gemella, Granulicatella, Neisseria, and Prevotella. They keep the balance right, stopping harmful bacteria from taking over. This helps prevent issues like cavities and gum disease.
The Role of Probiotics
Probiotics are live microorganisms that can be added to our mouths to balance the bacteria. Foods like kefir, sauerkraut, and shiitake mushrooms are rich in probiotics. Eating these can help keep our mouths healthy by changing the mix of microbes.
It’s important to keep a healthy mix of good bacteria in our mouths. This stops bad bacteria from growing too much and keeps our mouths balanced. By knowing about oral probiotics, we can support our oral health and lower the risk of diseases linked to an unbalanced microbiome.
“A healthy and balanced oral microbiome can help prevent dental problems, such as caries (cavities) and gum disease.”
| Beneficial Oral Bacteria | Benefits |
|---|---|
| Streptococcus | Helps maintain pH balance, inhibits harmful bacteria growth |
| Gemella | Produces antimicrobial compounds, contributes to immune function |
| Granulicatella | Assists in nutrient metabolism, supports enamel remineralization |
| Neisseria | Produces nitric oxide, promotes healthy gum tissue |
| Prevotella | Helps break down complex carbohydrates, maintains microbial diversity |
Harmful Oral Bacteria
The oral microbiome is always changing, but too many bad microbes can cause health problems. Streptococcus mutans, Porphyromonas gingivalis, and others are harmful bacteria. They include Tannerella forsythia, Aggregatibacter actinomycetemcomitans, Prevotella intermedia, Candida albicans, Fusobacterium nucleatum, and Treponema denticola.
These bad bacteria can lead to bad breath, plaque, tooth decay, and gum disease. When the balance in our mouths gets upset, these microbes can take over. This is called oral dysbiosis.
| Harmful Oral Bacteria | Associated Oral Health Issues |
|---|---|
| Streptococcus mutans | Tooth decay, cavities |
| Porphyromonas gingivalis | Gum disease, periodontitis |
| Tannerella forsythia | Gum inflammation, tooth loss |
| Aggregatibacter actinomycetemcomitans | Aggressive form of gum disease |
| Prevotella intermedia | Halitosis, bad breath |
| Candida albicans | Oral thrush, fungal infections |
| Fusobacterium nucleatum | Gum inflammation, link to colorectal cancer |
| Treponema denticola | Gum disease, tooth loss |
Knowing about these harmful oral bacteria helps us keep our mouths healthy. Good oral hygiene and fixing imbalances can stop these pathogens. This keeps us feeling good overall.
“Maintaining a diverse and balanced oral microbiome is essential for optimal oral and overall health.”
Common Harmful Oral Microbes
The human mouth is filled with many microorganisms, both good and bad. Streptococcus mutans and Porphyromonas gingivalis are two harmful bacteria that can harm our mouths.
Streptococcus mutans
Streptococcus mutans is a key cause of tooth decay. It feeds on sugars and turns them into acids that weaken tooth enamel. This leads to cavities. If not controlled, it can damage our teeth, causing pain and bad looks.
Porphyromonas gingivalis
Porphyromonas gingivalis is linked to periodontal disease, a serious gum issue. It lives in the spaces between gums and teeth, causing inflammation. This can make gums pull away and may lead to tooth loss if not treated. It disrupts the balance in our mouths, threatening our oral health.
Knowing about these harmful microbes helps us keep our mouths healthy. Good oral hygiene, regular dentist visits, and eating right can help keep them away.
Negative Health Effects of Harmful Microbes
The balance of microbes in our mouths is key to good oral health. But, harmful bacteria can cause bad breath, plaque, tooth decay, and gum disease.
Bad Breath
Bad breath, or halitosis, comes from gases made by harmful bacteria in our mouths. These bacteria hide in the mouth, tongue, and gums. They release smells that are hard to get rid of.
Plaque and Tartar Formation
Plaque, a sticky film of bacteria, forms on teeth if we don’t brush and floss regularly. It can turn into hard tartar over time. Tartar leads to cavities and gum disease.
Tooth Decay
Some bacteria, like Streptococcus mutans, make acids that weaken tooth enamel. This leads to cavities and tooth decay. If not treated, decay can badly damage teeth.
Gum Disease
Harmful bacteria cause gum disease, or periodontitis. It starts with gum inflammation and can destroy the bone and ligaments that hold teeth in place. This can lead to losing teeth.
To keep our mouths healthy, we must brush, floss, and use mouthwash like LISTERINE® Cool Mint. This helps kill up to 99.9% of harmful bacteria.
| Negative Health Effect | Percentage Impact |
|---|---|
| Percentage of adolescents in a clinical trial showing changes in oral microbiome due to fixed orthodontic appliances and fluoride mouthwash | 47% |
| Percentage impact on reducing periodontal disease by Lactobacillus brevis (CD2) treatment | 72% |
| Rate of reduction in caries process due to the complex oral microflora analysis in high-risk individuals | 17.3% |
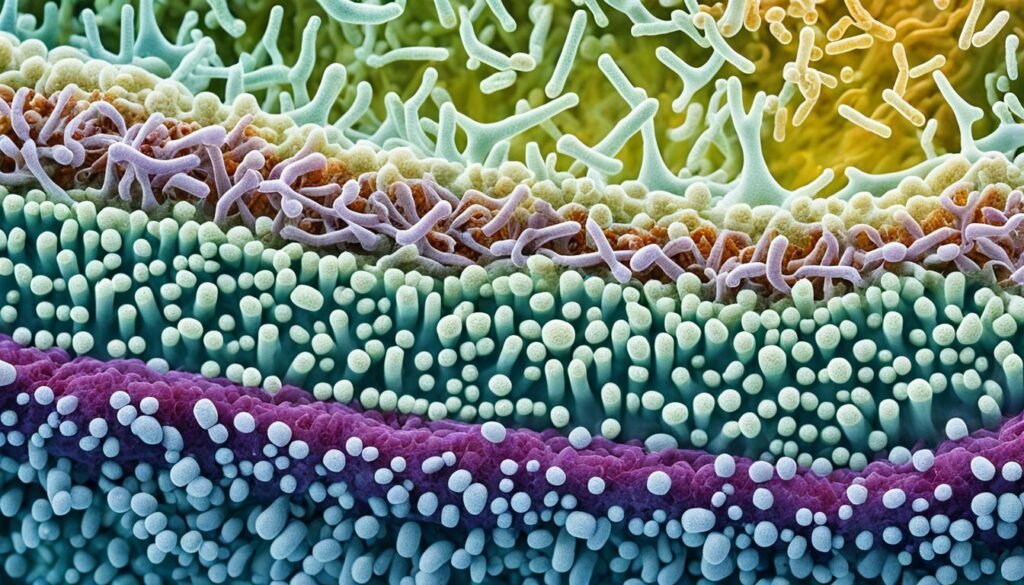
The Oral Microbiome Matrix
The human mouth is full of different bacteria. It has over 700 species living on teeth and the soft parts inside the mouth. These bacteria form a complex network called the oral microbiome. This network is key to keeping our mouths healthy.
Biofilms in the Mouth
Biofilms are at the center of the oral microbiome. They are thin layers of microorganisms that stick to surfaces in the mouth. These biofilms protect both good and bad bacteria, including dental plaque.
Dental plaque is a biofilm that builds up and can cause gum problems and tooth decay. The biofilm matrix feeds the bacteria, helping them grow and spread. This balance of bacteria in the biofilm is important for our oral health.
- The mouth has over 700 types of bacteria on teeth and soft tissues.
- The mouth has the second most diverse group of microorganisms in the body.
- About 80% of early biofilms in the mouth are made up of Streptococci.
- The bacteria in our mouths help keep us healthy by controlling harmful bacteria.
“The human body contains more prokaryotic organisms than eukaryotic cells, with only one out of 10 cells being human.”
Oral Microbiome and Overall Health
The oral microbiome is a group of tiny living things in our mouths. It’s key to our health. When it gets out of balance, with too many bad bacteria and not enough good ones, it can cause big problems.
Inflammation and Systemic Effects
Chronic inflammation from an unbalanced oral microbiome can lead to health issues. This includes cardiovascular disease, brain health problems like Alzheimer’s, diabetes, and obesity. Bad oral bacteria can get into the blood through inflamed gums. This can cause blood vessel inflammation and increase heart disease risk.
Cardiovascular Health Implications
The oral microbiome affects our heart health. Some oral bacteria are linked to atherosclerosis, which is plaque buildup in arteries. This can lead to heart attacks and strokes. Keeping the oral microbiome in balance is key for a healthy heart.
Brain Health Connections
Research is showing a link between the oral microbiome and brain health. An imbalance in the mouth can raise the risk of Alzheimer’s disease and other brain conditions. Scientists are studying the oral-gut-brain axis closely.
Diabetes and Insulin Resistance
People with diabetes and insulin resistance often have an unhealthy oral microbiome. This can make these conditions worse. Keeping the mouth healthy is crucial for managing these metabolic disorders.
Potential Links to Obesity
The oral microbiome might affect our gut and metabolism, leading to weight gain and obesity. Researchers are looking into how the oral and gut microbiomes work together. They want to understand how this affects our metabolism and weight.
In conclusion, the oral microbiome is a big part of our health. By keeping it balanced, we can support our body and lower the risk of many diseases.
Mapping the Oral Microbiome
Exploring the oral microbiome helps us understand our health and well-being. The Human Oral Microbiome Database (HOMD) is key in this journey. It’s a detailed database that highlights the many bacteria in our mouths.
The Human Oral Microbiome Database (HOMD)
The HOMD is a special 16S rDNA database. It offers info on about 700 main bacterial species in our mouths. It links sequence data with other info, helping researchers quickly identify oral bacteria.
This makes the HOMD crucial for understanding the oral microbiome and its health effects. Scientists use it to study the complex interactions in our mouths. The database shows how these bacteria work together and their roles in health and disease.
With the HOMD, researchers can dive into the world of mouth bacteria. It helps them understand the oral microbiome’s impact on health. This includes everything from dental issues to broader health problems.
| Key Statistics on Oral Microbiome Mapping | Findings |
|---|---|
| Genome-wide association study (GWAS) | Identified five genetic loci associated with the oral microbiota at study-wide significance. |
| Replication in independent cohort | Four out of the five associations were well replicated in an independent cohort of 1,439 individuals. |
| Variance explained by human genetics | Human genetics accounted for at least 10% of oral microbiome compositions between individuals. |
| Predictive power of microbiome and genetics | Machine learning models showed that polygenic risk scores dominated over the oral microbiome in predicting the risk of dental diseases such as dental calculus and gingival bleeding. |
| Relative impact of genetics and environment | Human genetics explain more variances of microbiome composition than environmental factors. |
The HOMD is a key tool for understanding the oral microbiome. It gives researchers and healthcare workers valuable data. This helps them improve our oral and overall health.
Oral Microbiome Analysis Methods
Studying the oral microbiome is key to understanding oral health. Traditionally, scientists used culture methods like microscopy and biochemical tests to find oral bacteria. But, about 31% of these bacteria can’t be grown in labs, limiting these old methods.
Culture Techniques
Culture methods have given us some insights, but they’re not complete. They can only find bacteria that grow in labs, missing most of the oral microbiome.
Molecular Methods
Then came molecular methods, like 16S rRNA gene sequencing, changing how we study the oral microbiome. These methods don’t need culturing to identify bacteria. They look at genetic signatures to understand the oral microbiome better.
The 16S rDNA sequencing is a top choice for studying the oral microbiome. It focuses on a specific part of the 16S ribosomal RNA gene. This lets researchers accurately identify and understand the diversity of oral bacteria.
| Method | Advantages | Limitations |
|---|---|---|
| Bacterial culture |
|
|
| Molecular methods (e.g., 16S rDNA sequencing) |
|
|
Using both culture-dependent and independent methods helps researchers understand the oral microbiome fully. This leads to better oral health care and disease prevention.
Site-Specificity of Oral Bacteria
The mouth is filled with many kinds of bacteria, each liking certain places better than others. These bacteria know exactly where to settle in the mouth. This shows how well they fit into their home.
Adhesins help guide oral bacterial colonization. Some bacteria love the tongue, while others do well on teeth or under the gumline. This oral bacteria site-specificity helps create a special order in dental plaque spatial organization. Anaerobic bacteria live in the middle, and aerobic ones on the outside, making a balanced community.
| Oral Niche | Predominant Bacteria |
|---|---|
| Tongue | Streptococcus, Actinomyces, Veillonella |
| Tooth Surfaces | Streptococcus mutans, Lactobacillus, Actinomyces |
| Subgingival Crevice | Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola |
These bacteria and their spots in the mouth help keep our mouths healthy. Knowing where they live is key to keeping the mouth balanced. This balance is important for good oral health.
“The spatial organization of oral bacteria within dental plaque is a testament to the intricate adaptations and interactions that have evolved over millennia.”
Understanding what bacteria like and where they live helps us keep the mouth healthy. This knowledge lets us find ways to keep the balance right, which is good for our health overall.
The Oral Microbiome and Disease
The oral microbiome is a complex mix of microbes in our mouths. It’s key to keeping our mouths healthy. But, when it gets out of balance, it can lead to oral diseases and affect our health overall. Researchers have found links between certain bacteria in our mouths and oral health issues and even some diseases.
Associations with Oral Diseases
Some bacteria, like Streptococcus mutans and Porphyromonas gingivalis, are linked to dental caries and other oral diseases. These harmful bacteria can upset the balance in our mouths. This can cause common oral health problems.
Oral Bacteria as Biomarkers
Research shows the oral microbiome could be a source of biomarkers for diseases. Studies link certain oral bacteria to pancreatic cancer, diabetes, and other diseases. The exact links are still being studied, but the oral microbiome is seen as a key to our health.
As we learn more about the oral microbiome and its role in health, using oral bacteria for diagnosis and treatment becomes more possible. Monitoring the oral microbiome could help spot early signs of disease. This could lead to better treatments for oral and overall health.
Conclusion
The oral microbiome is a complex ecosystem filled with many microorganisms. These microorganisms are key to keeping my mouth and overall health in check. It’s vital to understand how the oral microbiome works and the role of harmful bacteria to protect my health.
Keeping my oral microbiome balanced is crucial. This means practicing good oral hygiene like brushing and flossing regularly. Doing so helps prevent issues like bad breath, plaque, and gum disease. It also helps my overall health by reducing the risk of other diseases.
As I learn more about the oral microbiome, I can make better choices for my oral care. Using probiotics, prebiotics, and natural remedies helps support good bacteria and stop bad ones from growing. Keeping my oral microbiome healthy is key to protecting my teeth, gums, and overall well-being. It’s about taking a holistic approach to my health.
FAQ
Why is my oral health important for my overall health?
Your mouth health can affect your body’s health. Germs in your mouth can spread and cause infections. Without good oral care, these germs can lead to tooth decay and gum disease. Keeping your mouth healthy helps protect your overall health.
What is a microbiome?
A microbiome is a group of tiny living things that live in a specific place, like inside us. In our mouths, there are about 700 types of these tiny organisms, making up around 6 billion microbes.
What are some beneficial bacteria in the oral microbiome?
Good bacteria in our mouths include Streptococcus, Gemella, Granulicatella, Neisseria, and Prevotella. Probiotics can also add more good bacteria to our mouths.
What are some common harmful oral bacteria?
Bad bacteria in our mouths include Streptococcus mutans, Porphyromonas gingivalis, Tannerella forsythia, Aggregatibacter actinomycetemcomitans, Prevotella intermedia, Candida albicans, Fusobacterium nucleatum, and Treponema denticola.
How can harmful oral bacteria affect my health?
Bad mouth microbes can cause bad breath, plaque, tooth decay, and gum disease. They can also lead to inflammation, heart disease, brain health issues, diabetes, and obesity.
What is the Human Oral Microbiome Database (HOMD)?
The HOMD is a database that lists the about 700 main bacteria in our mouths. It helps researchers learn about the oral microbiome and its role in health and disease.
How do researchers study the oral microbiome?
Before, researchers used old methods to study oral bacteria. Now, new methods like 16S rRNA gene sequencing help us identify bacteria without needing to grow them in a lab.
How do oral bacteria colonize different parts of the mouth?
Bacteria in our mouths prefer certain places to live, based on how they stick to surfaces. This helps them arrange themselves in dental plaque.
How can the oral microbiome be used as an indicator of health?
Certain bacteria in our mouths are linked to oral health issues and diseases. They might also be signs of other diseases, like pancreatic cancer, diabetes, Crohn’s disease, heart disease, and preterm birth.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5122475/ – A practical guide to the oral microbiome and its relation to health and disease
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6503789/ – Oral microbiome: Unveiling the fundamentals
- https://www.rupahealth.com/post/oral-microbiome-101-understanding-the-basics-of-your-mouths-microbial-world – No title found
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10406501/ – Exploring the oral microbiome: an updated multidisciplinary oral healthcare perspective
- https://bio.libretexts.org/Bookshelves/Microbiology/Microbiomes_-_Health_and_the_Environment_(Parks)/03:_Human_Health_and_Disease/3.03:_The_Oral_Microbiome – 3.3: The Oral Microbiome
- https://biomcare.com/life-science/oral-microbiome/ – The oral microbiome | Its Importance and what is it?
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10048844/ – The Role of the Oral Microbiome in the Development of Diseases
- https://www.perionc.com/healing-your-oral-microbiome-a-pathway-to-a-healthier-mouth/ – Healing Your Oral Microbiome: A Pathway to a Healthier Mouth
- https://doctorstaci.com/learn/the-power-of-the-oral-microbiome/ – The Power of the Oral Microbiome – Doctor Staci – Healthy Teeth + Happy Lives
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9405223/ – Oral Microbiota, Its Equilibrium and Implications in the Pathophysiology of Human Diseases: A Systematic Review
- https://theconversation.com/the-bacteria-in-your-mouth-play-an-important-role-in-your-health-here-are-four-diseases-linked-to-your-oral-microbiome-230041 – The bacteria in your mouth play an important role in your health – here are four diseases linked to your oral microbiome
- https://www.periodontistphoenix.com/blog/oral-bacteria-and-its-impact-on-gum-health/ – Exploring Oral Bacteria and Its Impact on Gum Health
- https://www.nature.com/articles/s41368-022-00163-7 – Oral microbiota in human systematic diseases – International Journal of Oral Science
- https://www.sunstargum.com/gb-en/oral-health/oral-microbiome-guide-dental-patients.html – A Simplified Guide to Oral Microbiome and Why It Matters
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8457218/ – The oral microbiome: Role of key organisms and complex networks in oral health and disease
- https://newsinhealth.nih.gov/2019/05/mouth-microbes – Mouth Microbes
- https://www.listerine.com/fresh-breath/good-vs-bad-oral-microbiome-bacteria – The Oral Microbiome: Good vs. Bad Bacteria in Your Mouth | LISTERINE®
- https://www.nature.com/articles/sj.bdj.2016.865 – The oral microbiome – an update for oral healthcare professionals – British Dental Journal
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2768665/ – The Oral Microbiota: Living with a Permanent Guest
- https://www.nature.com/articles/s41579-023-00963-6 – The oral microbiome: diversity, biogeography and human health – Nature Reviews Microbiology
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6605021/ – Oral microbiome and health
- https://www.gutmicrobiotaforhealth.com/the-oral-microbiome-a-double-face-in-health-and-disease/ – The oral microbiome: a double face in health and disease
- https://www.nature.com/articles/s41421-021-00356-0 – Metagenome-genome-wide association studies reveal human genetic impact on the oral microbiome – Cell Discovery
- https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-020-01801-y – Defining the oral microbiome by whole-genome sequencing and resistome analysis: the complexity of the healthy picture – BMC Microbiology
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8125773/ – Oral–Gut Microbiome Axis in Gastrointestinal Disease and Cancer
- https://www.nature.com/articles/s41598-023-37246-2 – Factors influencing oral microbiome analysis: from saliva sampling methods to next-generation sequencing platforms – Scientific Reports
- https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2020.604596/full – Frontiers | Oral Microbiome Analysis in Prospective Genome Cohort Studies of the Tohoku Medical Megabank Project
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7153577/ – Biogeography of the Oral Microbiome: The Site-Specialist Hypothesis
- https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.895537/full – Frontiers | The Oral Microbiota: Community Composition, Influencing Factors, Pathogenesis, and Interventions
- https://www.nature.com/articles/s41522-021-00247-y – Periodontitis associates with species-specific gene expression of the oral microbiota – npj Biofilms and Microbiomes
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7074908/ – The Human Oral Microbiome in Health and Disease: From Sequences to Ecosystems
- https://www.mdpi.com/2076-2607/11/6/1453 – Oral Microbiome in Health and Disease: Maintaining a Healthy, Balanced Ecosystem and Reversing Dysbiosis
- https://www.mdpi.com/2076-2607/11/2/318 – The Contribution of the Human Oral Microbiome to Oral Disease: A Review
- https://www.georgetownsmile.com/blog/the-invisible-ecosystem-unveiling-the-wonders-of-the-oral-microbiome/ – The Invisible Ecosystem: Unveiling the Wonders of the Oral Microbiome
- https://www.researchednutritionals.com/a-healthy-oral-microbiome-the-key-to-systemic-health/ – A Healthy Oral Microbiome – Blog – Researched Nutritionals